A smooth, normal configuration of the macula is necessary to see clearly.
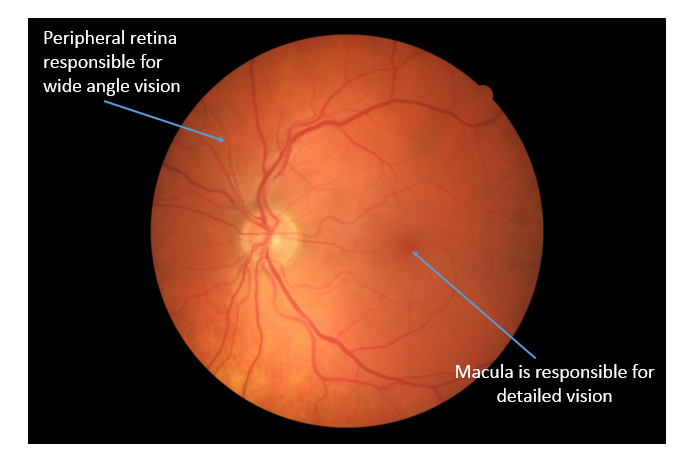
A smooth, normal configuration of the macula is necessary to see clearly. As we age, the vitreous gel that occupies the space in the middle of the eye liquefies and pulls away from the back of the eye. Sometimes, the gel has adherent attachments to the macula and does not pull away properly
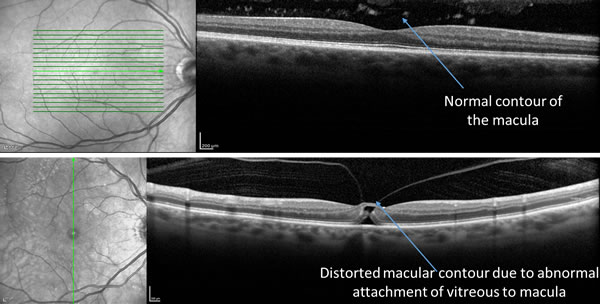
If very mild, vitreomacular traction syndrome can cause very little visual symptoms. If the condition is more severe, it can lead to traction on the macula which may result to distortion of vision.

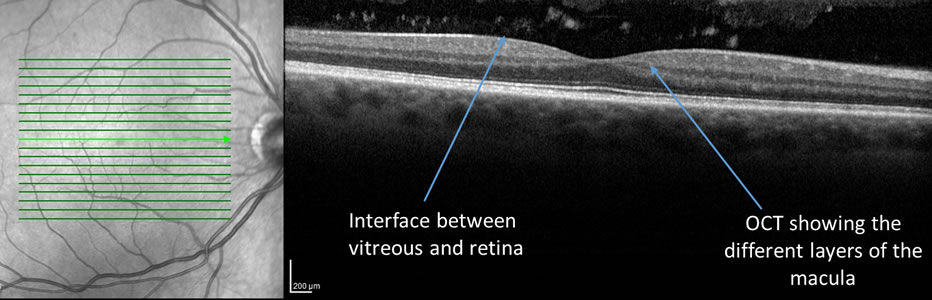
Vitreomacular traction syndrome can be detected with a thorough eye exam and an Optical Coherence Tomography (OCT). An OCT allows your ophthalmologist to get a “3-D biopsy” of the retina and study the interface of the macula and vitreous in great detail. Your ophthalmologist may also order further testing such as a fluorescein angiogram if needed. A fluorescein angiogram is a dye test that allows your ophthalmologist to evaluate for any leaking or new blood vessel formation in the retina.
If there are no symptoms, your ophthalmologist will likely follow you closely for vitreomacular syndrome. If there are visual symptoms such as distorted or decreased vision, treatment options such as surgery or medication can be discussed.
If mild, vitreomacular traction syndrome can be observed. Sometimes, the adherent vitreous will free itself and the macula will return to its normal position. The visual acuity after treatment of vitreomacular traction syndrome depends on how long it has been present and how severely it has impacted the retina. In some cases, vitreomacular traction syndrome can progress to a macular hole. In this case, surgery will likely be required.